

ASHP’s New Mentorship Program Advances Professional Development

Pharmacy Runs the Family: Siblings Follow in the Footsteps of their Pharmacist Parents

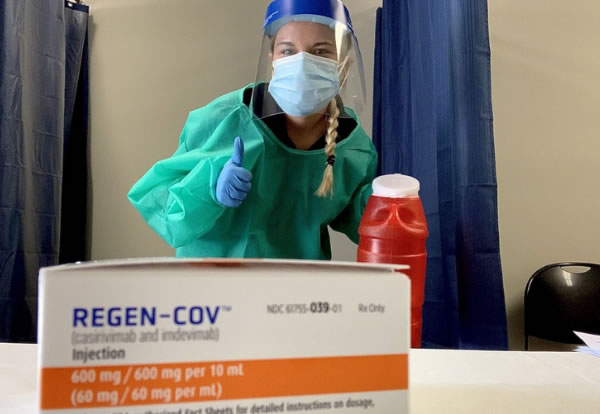
Pharmacy Technicians Find Rewarding Careers and Helpful Resources from ASHP
Community Pharmacy Residencies Offer Bounty of Opportunities




 If you want to contribute tutorials, news or other stuff please contact us. We pay 150 for each approved article.
If you want to contribute tutorials, news or other stuff please contact us. We pay 150 for each approved article. Consectetur adipisicing elit. Sed do eiusmod tempor incididunt ut labore.
Consectetur adipisicing elit. Sed do eiusmod tempor incididunt ut labore. This site uses valid HTML and CSS. All content Copyright © 2010 Newscast, Inc
This site uses valid HTML and CSS. All content Copyright © 2010 Newscast, Inc If you like what we do, please don't hestitate and subscribe to our
If you like what we do, please don't hestitate and subscribe to our